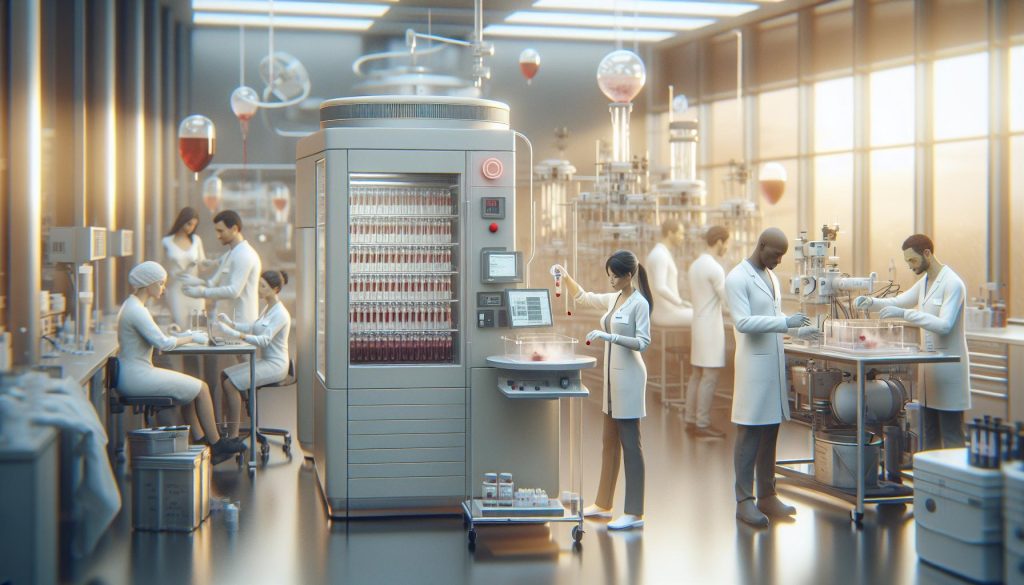
Did you know that the preservation of blood, vital for countless medical procedures, can be dramatically enhanced by cryogenic techniques? Cryogenic blood storage refers to the process of freezing blood components at extremely low temperatures, allowing for extended shelf life and viability. This innovative approach is not only crucial for emergency medicine and organ transplantation but also opens new frontiers in regenerative medicine and therapies for chronic diseases. As the demand for reliable blood supply continues to rise, understanding the applications and benefits of cryogenic blood storage becomes essential for both healthcare professionals and patients. Join us as we explore how this groundbreaking technology is reshaping the landscape of medical care and ensuring that lifesaving resources are always available when needed.
What Is Cryogenic Blood and Why It Matters
Cryogenic blood storage represents a revolutionary advancement in medical preservation, allowing blood and cellular components to be stored at extremely low temperatures, typically around -196°C (-321°F). This innovative technique is crucial for extending the shelf life of blood supplies, enabling life-saving transfusions, and improving the overall efficiency of blood banks. The process of cryogenic preservation minimizes cellular metabolic activity, effectively halting the deterioration of blood products and retaining their viability for future medical use.
The significance of cryogenic blood lies in its potential to address challenges in traditional blood storage methods, which typically have much shorter shelf lives-only a few weeks for red blood cells, for instance. With cryogenic methods, blood can be preserved for years, significantly alleviating shortages that often arise in blood donation programs. This extended preservation not only ensures that more patients have access to necessary treatments but also enhances the flexibility of blood usage in emergencies, surgeries, and specialized therapies.
Moreover, as research continues to illustrate the benefits of using cryogenics in other medical fields, the implications for regenerative medicine and transplant procedures become increasingly evident. Cryogenic processes can also be applied to stem cells and other cellular therapies, expanding the horizons of treatment options for various conditions. As the medical community explores these transformative applications, the promise of cryogenic blood storage is set to become a cornerstone in future healthcare innovations, fundamentally altering how we approach transfusion medicine and beyond.
The Science Behind Cryogenic Blood Storage
The preservation of blood at cryogenic temperatures opens up remarkable possibilities in medical science, making it an area of intense research and development. At the heart of cryogenic blood storage is the phenomenon of low temperatures significantly slowing down cellular metabolism. By cooling blood products to temperatures around -196°C (-321°F), the movement of molecules is drastically reduced, effectively halting biochemical reactions that lead to degradation and loss of viability. This preservation technique, known as cryopreservation, ensures that red blood cells, plasma, and other cellular components remain intact and functional over much longer periods compared to traditional blood storage methods.
Understanding the biological impacts of cryogenic temperatures is essential. When blood is frozen, ice crystals can form, which can damage cell membranes. To mitigate this risk, cryoprotectants-substances that inhibit ice formation-are added to the blood samples. Commonly used cryoprotectants include dimethyl sulfoxide (DMSO) and glycerol. These agents protect cells during the freezing and thawing processes, enabling higher cell survival rates post-cryopreservation. The successful application of these techniques relies not just on the cryogenic conditions but also on the careful preparation and handling of blood products, ensuring that both the cryoprotectants and freezing protocols are optimized for different cell types.
The implications of this technology extend beyond mere storage. By harnessing cryogenic blood preservation, healthcare systems can effectively manage blood supplies, especially in emergencies where timely access to viable blood products is crucial. In addition, the ability to store stem cells, which play a vital role in regenerative medicine, further underscores the potential for advancements in treatments for various diseases. As research continues to evolve, the chances of reviving previously unusable blood products after extensive storage periods will open new avenues for patient care, revolutionizing transfusion medicine and beyond.
In conclusion, not only addresses immediate challenges in blood supply management but also paves the way for transformative medical applications. The combination of low-temperature preservation and cryoprotectant technology creates a functional framework for the future of blood and cell storage, promising enhanced treatment options and improved outcomes for patients across a spectrum of medical needs.
Key Techniques for Cryogenic Blood Preservation
The art and science of cryogenic blood preservation are pivotal in modern medical practices, especially as the demand for viable blood products continues to grow. Employing several advanced techniques ensures that the integrity of blood and its components is maintained, allowing crucial medical procedures to operate smoothly even in cases of limited supply.
One fundamental technique is the use of cryoprotectants. These substances, such as dimethyl sulfoxide (DMSO) and glycerol, play an essential role in preventing ice crystal formation during the freezing process, which can damage sensitive cell membranes. When added to blood samples, cryoprotectants help maintain the structural integrity of red blood cells, platelets, and plasma. The concentration and method of introducing these agents can vary depending on the type of blood component being preserved, reflecting the importance of tailored approaches in maximising cell survival rates during both freezing and thawing processes.
Another vital aspect of cryogenic blood preservation is the controlled-rate freezing technique. Here, blood products are cooled gradually to reach optimal temperatures without inducing thermal shock that could compromise cellular viability. Utilizing specialized freezing equipment that carefully monitors and adjusts the cooling rate allows for a more homogenous lowering of temperature across the blood sample. This method helps ensure a minimal stress response from the cells, which is crucial for preserving function post-thaw.
Furthermore, advancements in storage protocols have proven indispensable. Cryogenic storage tanks, which maintain temperatures around -196°C (-321°F), are equipped with sophisticated monitoring systems that guarantee a consistent environment. These tanks often employ liquid nitrogen for optimal temperature regulation and minimize the risks associated with evaporation and temperature fluctuations. This meticulous control not only contributes to the long-term viability of blood products but also enhances the overall safety of the storage process.
As the field of cryogenic blood preservation evolves, ongoing research efforts are directed towards developing improved methods and technologies. Collaboration among medical professionals, researchers, and biotechnologists remains key to overcoming current challenges and pushing the boundaries of this valuable preservation technique, ultimately ensuring that cryogenic blood can play a transformative role in patient care and medical treatments.
Medical Applications of Cryogenic Blood
The ability to store blood at cryogenic temperatures opens up a world of possibilities for modern medicine, particularly in scenarios where immediate access to fresh blood products is critical. Cryogenic blood is particularly valuable in specialized treatments, including organ transplantation, cancer therapies, and advanced surgical procedures. By preserving blood and its components for extended periods, healthcare providers can ensure the availability of vital resources for patients whose needs may arise unexpectedly.
One of the primary medical applications is in the realm of transfusions, especially for patients with rare blood types. Cryogenically preserved blood offers a solution, enabling healthcare facilities to maintain sufficient supplies without the constant need for fresh donations. This is especially crucial in emergency situations such as trauma cases where time is of the essence. Moreover, specific components like platelets and plasma can be separated from whole blood and preserved individually, allowing for tailored treatments based on patient requirements.
In addition to transfusions, cryogenic blood finds its application in regenerative medicine and therapeutic procedures requiring stem cells. Blood contains hematopoietic stem cells, which play a vital role in regenerating blood and immune cells. By preserving these stem cells at cryogenic temperatures, clinicians can leverage their restorative capabilities for patients undergoing treatments for conditions like leukemia and other blood disorders. This innovative approach has significantly changed the landscape of treatment options available, giving hope to patients who previously had limited avenues for care.
Furthermore, research into cryogenic storage techniques is ongoing, with studies exploring optimal protocols to enhance the viability of stored blood components. For instance, advancements in cryoprotectant formulations are being investigated to provide better protection against cell damage during the freezing and thawing processes. Such innovations promise to not only extend the shelf life of cryogenically stored blood but also improve the outcomes of medical procedures that rely on these vital resources.
As the field progresses, the ethical implications and practical considerations surrounding cryogenic blood applications will also demand attention, ensuring that the benefits are maximized while minimizing any associated risks. Through careful research and ethical oversight, the potential of cryogenic blood storage may revolutionize how we approach medical treatments and patient care in the future.
Benefits of Using Cryogenic Blood in Treatments
The potential of cryogenic blood storage is revolutionizing modern medicine, opening up new avenues for patient treatment and care. One of the most significant benefits lies in its ability to extend the shelf life of blood products, making them readily available for transfusions, surgical procedures, and therapeutic interventions. By maintaining blood and its components at sub-zero temperatures, healthcare providers can overcome the limitations of traditional storage methods, which often lead to spoilage and waste.
Additionally, cryogenic blood storage plays a crucial role in treating patients with rare blood types. In emergencies, where time is of the essence, having access to preserved blood that matches a patient’s specific needs can be lifesaving. This technology ensures that even in the most critical situations, medical professionals can provide timely interventions. Furthermore, the ability to separate and store individual blood components-such as red blood cells, platelets, and plasma-allows for personalized treatment plans tailored to each patient’s unique medical situation.
The implications of cryogenic blood are also significant in regenerative medicine. Hematopoietic stem cells found in blood are vital for therapies aimed at blood disorders and conditions like leukemia. By cryogenically storing these cells, clinicians can utilize them effectively for transplants or therapies that rejuvenate the patient’s blood supply and immune system. Such advancements may improve patient outcomes and reduce the need for more invasive procedures.
Finally, the continuous research into optimizing cryogenic storage conditions and cryoprotectant formulations aims to maximize the viability of blood products. This ongoing innovation not only promises better preservation techniques but also enhances the overall safety and effectiveness of medical treatments reliant on these invaluable resources. As clinicians continue to explore the frontiers of cryogenic technology, the broader healthcare landscape stands to benefit, potentially saving countless lives and improving quality of care.
Challenges and Limitations of Cryogenic Blood Storage
The promise of cryogenic blood storage is tempered by several challenges that require careful consideration. One of the most significant hurdles is the management of cryoprotective agents. While these substances are essential for preventing ice crystal formation during the freezing process, their toxicity can pose risks to blood cells and tissues. The balance between effective cryoprotection and cytotoxicity must be meticulously maintained, and even slight deviations can lead to decreased viability of the stored blood components.
Another critical challenge is the technical requirements of cryogenic storage. Maintaining ultra-low temperatures, often below -150°C, demands sophisticated equipment and energy sources. Any failure in this system can lead to catastrophic consequences, including the loss of valuable blood products. Routine maintenance and monitoring systems are vital, but they also increase the operational costs associated with cryogenic blood storage facilities.
Furthermore, there are logistical implications tied to the transport and distribution of cryogenically preserved blood. Ensuring that blood products remain at optimal temperatures during transit can be complex, especially across different regions and healthcare facilities. The need for specialized containers and monitoring equipment can complicate logistics and inflate costs.
Lastly, the regulatory landscape presents its own set of challenges. Cryogenic blood storage falls under strict scrutiny by health authorities, necessitating comprehensive protocols for quality control and compliance. This regulatory burden can slow the adoption of new technologies and methods in blood preservation, limiting the potential benefits that cryogenic storage could offer.
In light of these challenges, ongoing research is crucial to mitigate these limitations and enhance the feasibility of cryogenic blood storage. Collaboration among researchers, healthcare providers, and regulatory bodies will be essential in overcoming these barriers, ensuring that the full potential of cryogenic blood storage is realized for the advancement of medical treatments.
The Future of Cryogenic Blood Technology
The advancements in cryogenic blood technology hold immense promise for the future of medical treatments, potentially revolutionizing how blood products are preserved and used. As research continues, several trends and innovations may shape this field, enhancing both the viability of cryogenically stored blood and its applications in various medical contexts.
One of the most significant advancements lies in the development of more efficient cryoprotective agents. These agents are crucial in preventing ice crystal formation during the freezing process, which can damage cells. Ongoing research is exploring biodegradable and less toxic options that could further enhance cell viability and reduce cytotoxic effects, making cryopreservation safer for transfusions and other medical uses. Improved formulations could significantly mitigate the challenges currently faced, allowing practitioners to store blood components longer without compromising quality.
Moreover, innovations in cryogenic storage equipment are poised to improve operational efficiencies. The integration of smart technology and artificial intelligence in monitoring systems can ensure precise temperature control and real-time data tracking, allowing for enhanced reliability in blood storage facilities. This technological advancement could minimize the risk of equipment failure during storage and transport, addressing one of the critical challenges identified previously.
As these technologies evolve, the potential applications of cryogenic blood storage in regenerative medicine and transplantation are also expanding. For instance, cryogenically preserved stem cells could help in the treatment of various conditions, from blood disorders to certain cancers, enhancing the pool of available options for patients. Additionally, collaborations between cryogenics experts and medical professionals are likely to yield new techniques that could make cryogenic blood a standard practice in more healthcare settings, further bridging the gap between research and clinical application.
In summary, is bright, characterized by innovative solutions aimed at enhancing safety, efficacy, and accessibility. As healthcare continues to embrace cutting-edge technologies, the promise of cryogenically preserved blood is becoming more achievable, though it remains essential for all advancements to be backed by rigorous research and clinical validation. Engaging in this field may pave the way for groundbreaking treatments, benefitting patients and healthcare providers alike.
Ethical Considerations in Cryogenic Blood Use
The rise of cryogenic blood storage technology opens up a complex landscape of ethical considerations that demand careful thought and discourse. As this method garners attention for its potential to improve medical treatments, it raises questions around consent, usage, and the implications of long-term preservation of human biological materials. One of the foremost concerns is the need for informed consent from donors. Stakeholders must ensure that individuals providing blood for cryogenic storage fully understand the risks, benefits, and long-term implications of their contributions. This includes being aware of how their blood may be used in future medical interventions or research.
Another significant ethical aspect involves the equitable access to these advanced technologies. There is a risk that cryogenic blood storage could widen existing disparities in healthcare. Access to innovative therapies often depends on socioeconomic status, leading to a situation where only certain populations can benefit from the advancements that cryogenic blood technology offers. Ensuring equitable access is not just a matter of ethics; it is also crucial for fostering trust in medical systems and innovations. Efforts should be made to develop policies that uphold fairness and justice in the application of these technologies across diverse demographic groups.
Furthermore, the implications of cryogenically preserved blood in research and treatment raise questions about the commodification of biological materials. As the demand for blood products increases, there may be ethical dilemmas surrounding the commercialization of blood storage and the potential exploitation of vulnerable populations. Scenario planning and regulatory frameworks could play an essential role in navigating these concerns, ensuring that the pursuit of innovation does not come at the expense of ethical integrity.
Finally, the long-term storage of biological materials brings forth considerations about the future of these samples. Questions about ownership, rights to withdraw consent, and the potential for genetic information to be harvested or misused are critical. As such, robust policies need to be established to protect the interests and rights of donors while fostering an environment of ethical research practices. Addressing these ethical considerations is vital for paving the way to widespread acceptance and trust in cryogenic blood technology, ensuring that its deployment ultimately serves the greater good in medical science and patient care.
Cryogenic Blood Storage vs. Traditional Methods
The evolution of blood preservation techniques marks a significant milestone in medical science, with cryogenic blood storage emerging as a pioneering option. Traditional blood storage methods typically involve refrigeration at temperatures between 1-6°C, allowing for preservation for up to 42 days. However, these standard methods face limitations in both storage duration and the preservation of cellular integrity. As a result, when blood is stored using these methods, it gradually loses viability, compromising its effectiveness for transfusions and medical treatments.
Cryogenic blood storage, on the other hand, utilizes ultra-low temperatures, typically around -196°C using liquid nitrogen, to achieve significantly longer preservation times. This method minimizes cellular metabolism and slows down biochemical processes, effectively halting degeneration. The advantages of cryogenic storage include the potential to preserve blood for years while maintaining the functional characteristics of red blood cells, platelets, and plasma proteins. The implications of this are profound, notably for transplant medicine, where the availability of high-quality blood products can greatly enhance patient outcomes.
Key Differences
Understanding the differences between cryogenic blood storage and traditional methods is crucial for appreciating their respective benefits:
- Storage Duration: Traditional methods allow for preservation for just a few weeks, while cryogenic techniques can extend this to several years.
- Cellular Integrity: Cryogenic storage maintains cellular structures in their original state, ensuring better functionality upon thawing compared to refrigerated blood.
- Cost and Infrastructure: While cryogenic systems can require more investment in technology and training, they provide greater efficacy that can reduce costs associated with short shelf life in traditional methods.
- Specialized Applications: Cryogenically stored blood can be especially beneficial for rare blood types or in situations where blood is needed for specialized procedures, providing a more reliable resource.
Shifting from traditional blood storage to advanced cryogenic methods not only addresses the limitations of existing practices but also opens new possibilities in medical applications, including enhanced treatments for trauma and surgical patients. As the field continues to evolve, so do the prospects for improved patient care and improved outcomes for those in need of blood transfusions and other blood-related treatments.
Real-Life Success Stories of Cryogenic Blood Applications
Advancements in cryogenic blood storage have not only revolutionized the field but also paved the way for some remarkable real-life success stories that showcase its potential in medical applications. One particularly compelling example comes from transplant medicine. In a notable case, a patient in need of a rare blood type faced a critical delay in receiving a compatible transfusion. Using cryogenically preserved blood, healthcare providers were able to access a stock of AB-negative blood that had been stored for over two years. This timely intervention significantly improved the patient’s chances of recovery and exemplified how cryogenic methods can provide a vital lifeline, particularly when rare blood types are required.
Another inspiring instance is found in the realm of regenerative medicine. In a study exploring the use of cryogenically stored platelets for surgical procedures, researchers discovered that thawed platelets maintained an impressive functional capacity, leading to enhanced postoperative recovery outcomes in patients undergoing major surgeries. The ability to preserve platelets at ultra-low temperatures for extended periods not only improved surgical protocols but also reduced the operational burden on blood banks, allowing for better resource management.
Additionally, cryogenic blood solutions have been utilized in emergency medical scenarios, such as in military operations. One success story involves a battlefield hospital where access to fresh blood supplies is often limited. By employing cryogenically preserved blood products, practitioners were able to quickly administer transfusions to injured soldiers, thereby saving lives that might have been lost due to delays in obtaining fresh blood.
These case studies underline the transformative impact of cryogenic blood storage in real-world settings. As this technology continues to develop, the medical community is increasingly recognizing its potential to enhance patient care and outcomes across various disciplines. Always consult with qualified healthcare providers for personalized advice and treatment options, particularly regarding cryogenic techniques and their application in specific medical situations.
Comparative Analysis of Cryogenic Blood Solutions
Cryogenic blood storage presents a groundbreaking advancement in the management of blood supplies, particularly vital for situations demanding rare blood types or significant quantities of blood products in emergencies. The comparison between various cryogenic blood solutions reveals significant differences in methodology, efficacy, and application, ensuring healthcare providers can make informed decisions tailored to specific medical needs.
A principal area of distinction lies in the preservation techniques employed for blood products. Two predominant methods are liquid nitrogen storage and vapor phase storage. Liquid nitrogen storage offers ultra-low temperatures (-196°C), ensuring long-term viability for red blood cells, platelets, and plasma. This method is often favored for its ability to inhibit cellular and biochemical degradation. On the other hand, vapor phase storage provides slightly higher temperatures while still maintaining cryogenic conditions. Although it is less efficient for some tissues, it allows for easier handling and reduces the risk of cryogenic burns during daily operations, making it a practical option for many facilities.
In terms of processing and thawing protocols, cryogenically stored blood can differ significantly. Standardized protocols ensure that thawed blood maintains cell integrity and function, which is crucial for effective transfusions. For instance, studies have shown that thawed red blood cells can retain their oxygen-carrying capacity for an extended period, while platelets can be effectively used even after prolonged cryopreservation, impacting surgical and emergency procedures positively. The comparative success rates of these processes underscore the importance of adhering to specific guidelines, which ultimately influence patient outcomes.
Furthermore, the medical applications of cryogenic blood solutions extend beyond emergency transfusions. They are increasingly utilized in regenerative medicine and advanced surgeries, where the availability of functional blood products can enhance procedural outcomes. The unique characteristics of cryogenically preserved blood enable healthcare providers to deploy specific components only as necessary, thus improving resource management and cost efficiency.
In conclusion, understanding the equips medical professionals and blood banks with the knowledge required to optimize blood usage effectively. The evolution of cryogenic technologies continues to pave the way for better patient care, addressing critical needs in diverse medical scenarios. Always consult with healthcare experts to establish the best practices for utilizing these innovative storage solutions in treatment plans.
Getting Involved: Donor and Research Opportunities
Engaging in cryogenic blood initiatives not only contributes to advancing medical technology but also plays a crucial role in enhancing patient care during emergencies. With the potential for cryogenic storage to extend the viability of blood products significantly, the demand for donors who are willing to participate in this innovative area is increasing. As a potential donor, you enable medical professionals to access rare blood types and manage critical situations more effectively.
There are also numerous research opportunities available for those interested in the science behind cryogenic blood preservation. Many universities and hospitals conduct studies aimed at improving storage techniques and the clinical applications of cryogenically preserved blood. Participating in these studies can involve everything from laboratory research to clinical trials, providing valuable insights that may lead to breakthroughs in transfusion medicine and regenerative therapies. Collaboration with research teams can also open the door to exchanging ideas and innovations that benefit the wider medical community.
Consider supporting these programs through various initiatives. Many organizations actively seek volunteers for blood donation drives, especially those focusing on rare blood types or specific medical conditions requiring cryogenic blood products. In addition, educational outreach programs aim to raise awareness about the importance of cryogenic preservation. Engaging in community discussions or educational workshops can help spread knowledge and garner support for this evolving field.
Ultimately, whether as a donor or a researcher, getting involved in cryogenic blood initiatives not only enhances personal knowledge but also contributes to a larger mission of improving medical outcomes and patient care. Stay informed through healthcare providers or local blood banks about how you can contribute and benefit from the advancements in cryogenic blood technology while ensuring that all participation aligns with ethical standards and clinical best practices.
FAQ
Q: What is the process of cryopreservation for blood?
A: Cryopreservation involves lowering the temperature of blood to preserve its cellular components for long-term storage. The blood is typically mixed with a cryoprotectant to prevent ice crystal formation, then cooled gradually to sub-zero temperatures. This method allows for storage of red blood cells, plasma, and platelets, maintaining their functionality upon thawing.
Q: How long can cryogenically stored blood be preserved?
A: Cryogenically stored blood can be preserved for years, with red blood cells lasting up to 10 years or more under optimal conditions. Plasma can be stored for several years, while platelets are typically viable for a shorter duration, around 5-7 days once thawed. Always ensure proper storage protocols are followed for best outcomes.
Q: What are the main advantages of using cryogenic blood storage?
A: The main advantages include long-term preservation of blood components, reduced waste due to spoilage, and the ability to store large quantities of blood in minimal space. Cryogenic storage also allows for the preservation of rare blood types, which can be vital for emergency medical situations.
Q: Are there any risks associated with cryogenic blood storage?
A: Yes, risks include potential damage to cells during freezing and thawing cycles, as well as contamination if proper sterile techniques are not employed. Additionally, the long-term effects of cryoprotectants on blood components require ongoing research to ensure safety and efficacy.
Q: What are the limitations of cryogenic blood storage compared to traditional methods?
A: Limitations include higher costs associated with cryogenic technology and the complexity of the equipment needed for maintaining ultra-low temperatures. Additionally, there might be concerns regarding the efficacy of revived cells compared to freshly collected blood under traditional methods.
Q: How is cryogenic blood used in medical treatments?
A: Cryogenic blood is utilized in various medical treatments, including transfusions for trauma patients, surgeries, and chronic conditions requiring frequent blood supply. It is particularly valuable for patients with rare blood types or those needing specific blood components like stem cells.
Q: What ethical considerations exist around cryogenic blood storage?
A: Ethical considerations include concerns about consent for blood donation, the handling of genetic material in stored blood, and issues related to possible commodification of blood products. Ongoing discussions in medical ethics address how to best manage these concerns while advancing medical technology.
Q: How does cryogenic blood storage impact future transplantation options?
A: Cryogenic blood storage significantly enhances future transplantation options by enabling the long-term preservation of donor organs and components, increasing availability, and improving matching processes. As technology advances, it may lead to more successful transplant outcomes and better resource management in medical facilities.
In Conclusion
Understanding cryogenic blood storage opens new avenues in medical applications, enhancing the potential for life-saving treatments. By leveraging advanced storage techniques, we can ensure the viability of blood for critical medical procedures. If you’re curious about the latest innovations in medical technologies or want to deepen your knowledge on topics like hematology or regenerative medicine, explore our related articles on blood preservation methods and developments in cryogenics.
Don’t hesitate-get involved by joining our newsletter for insights and updates that can keep you informed about the future of medical applications. Share your thoughts in the comments below or reach out for any questions you may have. As you continue your exploration, remember that understanding these advancements could lead to profound impacts on patient care. Embrace the journey of knowledge today, and keep discovering what’s next in healthcare innovation!